- From the Field
- Are GLP-1s the next industry disruptor?
- Some are predicting that GLP-1s could pose a disruptive threat to the medtech industry, as demand for medical devices and surgical procedures could be greatly reduced.
- 2024-07-24 13:44
- Key Insights
-
- While GLP‑1s have been around almost 20 years, they’ve recently been catapulted into the public domain due to their demonstrated effectiveness as a weight loss agent.
- This success has led to speculation about broader impacts on the medtech industry, given its principal role in the treatment and management of obesity and its comorbidities.
- Some are predicting that GLP‑1s pose a disruptive threat to the medtech industry, as demand for medical devices and surgical procedures could be greatly reduced.
The rise of glucagon‑like peptide‑1 receptor agonists—aka GLP‑1s—in recent years, has been meteoric. While GLP‑1s have been around almost 20 years, initially approved as a treatment for type 2 diabetes, they’ve recently been catapulted into the public domain due to their demonstrated effectiveness as a weight loss agent. This success has naturally led to speculation about broader impacts on obesity comorbidities, such as diabetes, heart disease, sleep apnea, and orthopedics—areas for which medical devices and surgical procedures are the principal means of management and treatment. Some commentators are already predicting that GLP‑1s could disrupt the medtech industry, potentially reducing demand for devices and surgeries significantly. Certainly, GLP‑1s have transformative potential, but, for all their promise, we do not expect them to replace medical devices or surgical procedures entirely. In this paper, we consider the recent surge in popularity and prevalence of GLP‑1s, the associated complexities, and the potential impacts on key areas of the medtech industry.
Understanding the rapid rise of GLP‑1s
To appreciate the sharp increase in popularity of GLP‑1 therapies in recent years, it is important to understand that obesity is one of the largest threats to public health in the world today. The World Health Organization defines adult obesity as a body mass index (BMI) greater than or equal to 30, and the latest data show that there were 890 million adults living with obesity worldwide in 2022.1 This is a global epidemic, one that has increased exponentially over recent decades and continues to rise.
Global obesity continues to rise
This is a worldwide epidemic and a major threat to public health
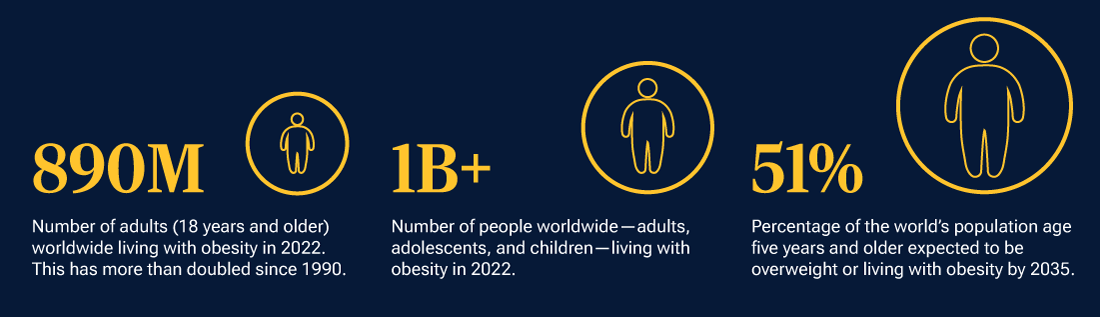
Latest data update as of February 28, 2024.
Source: World Health Organization.
In the context of this significant and growing global risk, effective weight loss therapies are health care’s holy grail and go a long way toward explaining the excitement surrounding GLP‑1s. The therapies function by mimicking the action of the body’s natural GLP‑1 hormone, suppressing appetite, contributing to better management of blood sugar levels, and aiding weight loss (Fig. 1).
The physiological impact of GLP‑1s
(Fig. 1) GLP‑1 mechanism of action when blood sugar levels increase
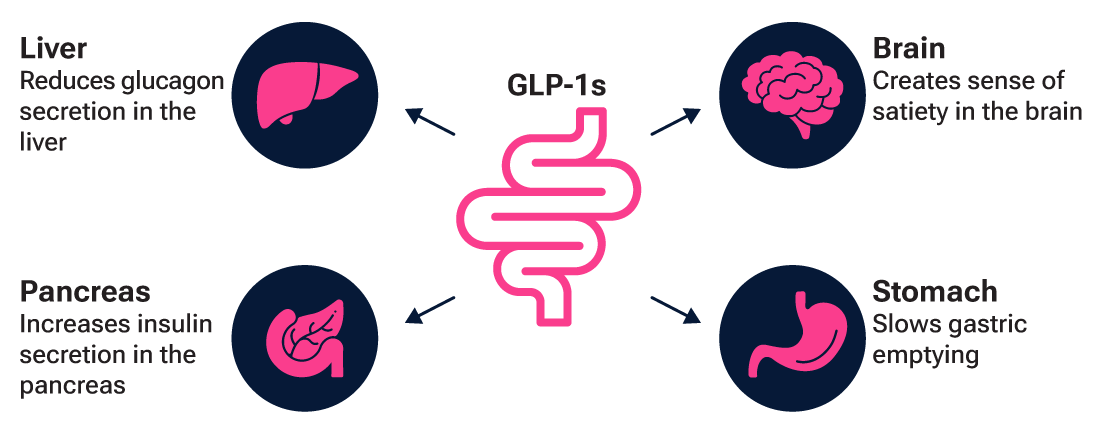
Source: Novo Nordisk investor presentation 2022.
Indeed, it is the efficacy of GLP‑1s in reducing weight that has recently catapulted them into the public domain. Results of a pivotal clinical trial conducted by Novo Nordisk in 2020 showed patients losing an average 14.9% of body weight within 68 weeks of commencing the once‑weekly dosage (Fig. 2).2 Patient uptake data further underscore this effectiveness, with GLP‑1 prescriptions increasing by a massive 300% between 2018 and 2023.3
Impacts and implications for the medtech industry
The success of GLP‑1s in clinical trials has seen companies within the medtech industry come under pressure, particularly those specializing in diabetes and obesity management. Indeed, the last half of 2023 proved a tumultuous time for medtech companies amid concerns that increasing GLP‑1 adoption will dramatically reduce the need for medical devices and surgical interventions. Confidence was undermined in June 2023, for example, when the American Diabetes Association presented evidence confirming the effectiveness of GLP‑1s in managing diabetes and achieving weight loss. The pivotal moment for the medtech industry, however, occurred in August 2023, when further clinical trial results from Novo Nordisk revealed a notable reduction in cardiovascular events in patients receiving GLP‑1 therapies. This announcement sparked a sharp sell‑off in medtech companies, with the industry ultimately falling almost 30% during the final three months of the year.
In trying to understand the potential longer‑term impact of GLP‑1s on the medtech industry, it is important to define what we know about GLP‑1s to date and what remains unclear. While they are certainly impactful, the excitement surrounding GLP‑1s clouds the fact that there is still much that is unknown about their safety and effectiveness as a long term weight loss agent. The risk is amplified by the fact that GLP‑1 drugs as a weight loss therapy have not followed the usual methodical rollout of new drug therapies. Their popularity is less attributable to physician enthusiasm, and more to overweight people looking for a “wonder drug” to fix a complicated health issue.
GLP‑1s—Demonstrated highly effective weight loss agent
(Fig. 2) Pivotal clinical trial showed an average of 14.9% weight loss
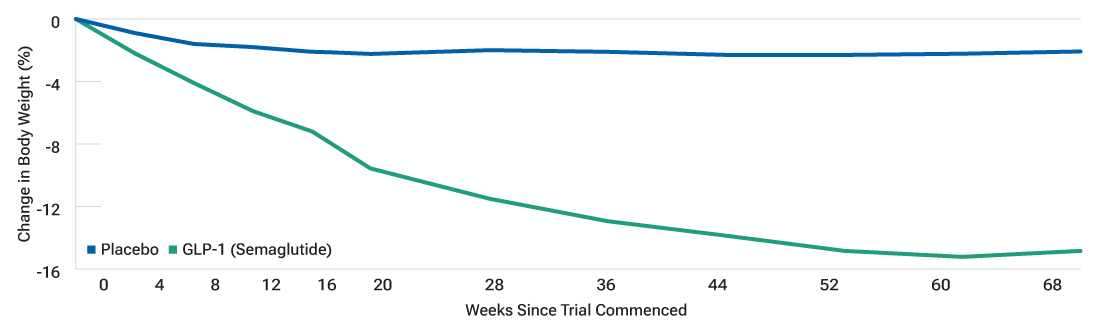
As of June 4, 2020.
Source: Novo Nordisk, STEP 1 clinical trial data.
What we know
We know that GLP‑1s treat weight loss and type 2 diabetes effectively. We know that obesity and type 2 diabetes have many comorbidities. We know that access to these drugs is limited currently but should improve in the coming years. We also know that demand is very strong and growing.
What remains unclear
- Access: We don’t know how many people will ultimately be on these drugs at any given time. Given capacity and reimbursement constraints, we estimate that around 2% of the U.S. population will be on GLP‑1s in 2024, and potentially rising to 6% of the U.S. population by 2028. Indeed, further positive clinical trial results recently make it more likely that payers will cover the cost of these drugs, potentially alleviating some of the reimbursement barriers and increasing access over time.
- Compliance: We have seen many different data points on patient compliance with the drugs—we will learn a lot more in the coming years as we see how many of the current patients stay on the drugs and what happens when they come off of them.
- Durability: We have seen some data on durability of weight loss after stopping the drug—we do not yet know the durability in real life.
- Patient impacts: The ultimate impact on the health care system will be determined by the number of patients taking the drugs (combination of access, durability, and compliance), as well as the impact on comorbidities. We are still learning the impact of GLP‑1s both on comorbidities with obesity and type 2 diabetes as well as other medical conditions, such as knee osteoarthritis. We are beginning to see the impact in trials; we do not yet know the impact in real‑world experience. Patient behavior in the real world frequently differs from patient behavior in trials.
Implications for specific medtech areas
The medical establishment historically has been slow to change guidelines and practices. In our discussions with dozens of doctors over the past year, most expect little to no impact on long‑term surgical volumes beyond the possible exception of bariatrics. While these perspectives should be taken with a grain of salt, as doctors are not always the first to see change coming, it is noteworthy just how different the tone is within the investment community—versus the medical community—around weight loss drugs. The majority of doctors we have spoken to do not believe that enough patients will consistently take GLP‑1s—or that the drugs will cure other medical conditions—to the point where it impacts surgical volumes in any significant way.
To understand the potential impact on patient populations in key areas of the medtech industry, it is important to consider these through the lens of GLP‑1 application/utilization:
- Bariatric surgery: Medtech companies that make devices related to bariatric surgery for weight loss should anticipate that physicians will aim to exhaust nonsurgical options. This will likely impact demand for bariatric devices.
- Orthopedics: Weight loss may reduce the wear and tear on joints, but more active and able patients will potentially increase demand for knee and hip replacements. People without obesity will continue to need joint replacements at the same rate as before.
- Cardiovascular devices: Evidence is mounting that GLP‑1s can lower incidence of heart attacks and strokes. A recent Novo Nordisk clinical trial found that overweight or obese adults with established heart disease taking GLP‑1 medication experienced a 20% reduction in cardiovascular events.4 While these trial results are encouraging, it is important to distinguish between relative risk reduction and absolute risk reduction. As exciting as the cardiovascular effects are, the absolute change in the number of patients who will have a cardiovascular event over time is not such a significant number. Meanwhile, the impact on cardiology practice remains to be seen. Current medical industry sentiment suggests that stents, pacemakers, and other devices will likely continue to be widely used.
- Diabetes: GLP‑1s have been prescribed for diabetes for almost two decades (since the first U.S. Food and Drug Administration approval in 2005). Devices such as continuous glucose monitors have not only continued to be used, their prevalence has risen, and they are increasingly used by individuals with prediabetes.
- Sleep apnea: Obesity is the main risk factor for obstructive sleep apnea, raising the possibility that weight loss may reduce incidence of this disorder, along with the need for continuous positive airway pressure (CPAP) devices. Certainly, the relationship between weight and sleep is complicated—poor sleep quality definitely impacts weight loss and gain. However, this is one area where GLP‑1s could actually have a game‑changing impact. Recent clinical trial data also adds support to this view.
Medtech innovation and product advancement are exciting
Significantly, the medtech industry has bounced back in 2024. Despite the panic expressed in the markets towards the end of 2023, utilization rates remain strong and patient volumes for both devices and surgical interventions have not been materially impacted. Over a longer‑term horizon, certain areas within medtech will continue to feel pressure from the rising prevalence of GLP‑1s, particularly as access, utilization, and cost reimbursement rates increase over time. However, we continue to be positive about the longer‑term outlook for the medtech industry, in general. The innovation and product cycle, which has historically been a key driver of medtech industry growth, looks particularly exciting. Advances in artificial intelligence‑enabled products, device miniaturization, and robotics are just some of the areas that can potentially fuel significant improvements in patient treatment and quality of life.
"The innovation and product cycle, which has historically been a key driver of medtech industry growth, looks particularly exciting."
In summary, penetration of GLP‑1 therapies is expected to continue, but long‑term use will depend on patient adherence, safety, and cost. While the potential of GLP‑1 drugs is very promising, we do not expect them to replace medical devices and surgical procedures entirely, particularly given the innovation and product advancement that are defining features of the medtech industry. Accordingly, the future will most likely see a coexistence of GLP‑1 therapies, medical devices, and surgical procedures with each playing an integral and collaborative role in patient care.
Get insights from our experts.
Subscribe to get email updates including article recommendations relating to global equities.
-
1Source: World Health Organization. Latest data update as of February 28, 2024.
2Novo Nordisk, as of June 4, 2020.
3Trilliant Health: 2023 Trends Shaping the Health Economy Report. As of September 27, 2023.
4The New England Journal of Medicine, November 11, 2023.
-
Important Information
This material is provided for informational purposes only and is not intended to be investment advice or a recommendation to take any particular investment action.
The views contained herein are those of the authors as of July 2024 and are subject to change without notice; these views may differ from those of other T. Rowe Price associates.
This information is not intended to reflect a current or past recommendation concerning investments, investment strategies, or account types, advice of any kind, or a solicitation of an offer to buy or sell any securities or investment services. The opinions and commentary provided do not take into account the investment objectives or financial situation of any particular investor or class of investor. Please consider your own circumstances before making an investment decision.
Information contained herein is based upon sources we consider to be reliable; we do not, however, guarantee its accuracy. Actual outcomes may differ materially from any forward‑looking statements made.
Past performance is not a reliable indicator of future performance. All investments are subject to market risk, including the possible loss of principal. All charts and tables are shown for illustrative purposes only.
T. Rowe Price Investment Services, Inc., distributor, and T. Rowe Price Associates, Inc., investment adviser.
© 2024 T. Rowe Price. All Rights Reserved. T. ROWE PRICE, INVEST WITH CONFIDENCE, and the Bighorn Sheep design are, collectively and/or apart, trademarks of T. Rowe Price Group, Inc.
202407‑3733946